Cardiac Insufficiency Treatment
Introduction
Stem cells are considered as the building blocks of life. These cells have the remarkable potential for regeneration and development into various different cell types in the body during early life and growth.
Stem cell therapy involves the use of stem cells for regeneration of the diseased and damaged tissues or organs to improve the quality of life of people suffering from various incurable diseases.
Newer and advanced regenerative medicines can use stem cells to create living and functional tissues. This can help to regenerate and repair tissue and organs in the body which are damaged due to age, disease and congenital defects. Stem cells have the power to migrate selectively to these damaged areas and develop into new cells and tissues by performing a repair and a renewal process. This can possibly result in anatomical as well as functional restoration. Regenerative medicine has the potential to provide a cure for failing or impaired tissues.
Regenerative medicine is an emerging branch of medicine with the goal of restoring organ or tissue function for patients with serious injuries or chronic disease. In these cases, the body’s own responses are not sufficient enough to restore functional tissue. A growing crisis in organ transplantation and an aging population due to advances in medical field have driven a search for new and alternative therapies. There are thousands of patients who are in the transplant-waiting list in each major hospital. In addition there is a wide range of major unmet medical needs which might be addressed by regenerative technologies.
Iranian scientists have moved to the forefront in embryonic stem cell research, according to a recent joint study by Harvard University and the Massachusetts Institute of Technology
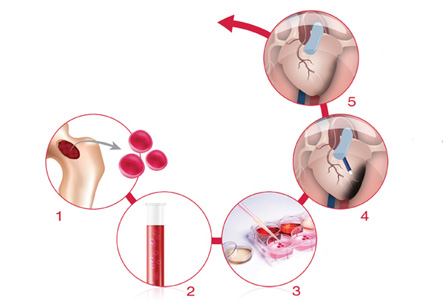
Treatment of Cardiac insufficiency with stem cells
Several clinical trials have been conducted targeting heart diseases which show that the adult stem cell therapy is safe, effective, and equally efficient in treating old and recent myocardial infarcts. Although initial studies demonstrated remarkable therapeutic effects, later clinical trials achieved only modest, but statistically significant improvements. Possible reasons for this discrepancy in results are patient age, timing of treatment and the recent history of a myocardial infarction. These obstacles may be overcome by additional treatments on the transplanted stem cells or the patient which can increase the effectiveness of the treatment. Refining the technology can further improve the results. Current studies vary greatly in cell harvesting techniques, cell types, cell administration timing and procedures, and also the studied parameters. This makes it very difficult to standardize the results and make comparisons. Comparative studies are therefore currently needed.
Stem-cell therapy for treatment of myocardial infarction usually makes use of autologous bone marrow stem cells. However, other types of adult stem cells may also be used, such as adipose-derived stem cells. Adult stem-cell therapy for treating heart disease was available in at least five continents from 2007.
Possible mechanisms of recovery include:
• Generation of new heart muscle cells
• Stimulation of growth of new blood vessels to re-establish the circulation in damaged heart tissue
• Secretion of growth factors
• Additional unknown mechanisms
• It may be possible to have adult bone marrow cells differentiate into heart muscle cells.
Several clinical trials have been conducted targeting heart diseases which show that the adult stem cell therapy is safe, effective, and equally efficient in treating old and recent myocardial infarcts.
The first successful integration of human embryonic-stem-cell-derived cardiomyocytes in lab animals was reported by researchers in August 2012. The contraction strength of muscles was measured four weeks after the guinea pigs were subjected to stimulated heart attacks and cell treatment. The new cells contracted synchronously with the existing cells. But it is unknown if the positive results were produced mainly from paracrine (by secreting factors) as opposed to direct electromechanical effects from the human cells. Future works are needed for determining how the cells can be engrafted more strongly around the scar tissue. Whether treatments from embryonic or adult bone marrow stem cells will prove more effective remains to be seen?